This article is part of an ongoing series about my Spontaneous Bilateral Patellar Tendon Rupture incident and knee surgery as a patient with Lupus, other chronic diseases and steroid therapy. Each part of the series will be updated and can be referenced below:
Disclaimer: This article is meant for educational purposes and is based on the author’s personal experiences. It is not to be substituted for medical advice. Please consult your own doctor before changing or adding any new treatment protocols.
Pin to Your Knee Surgery & Chronic Illness Boards:

Table of Contents
Week 1: Post Knee Surgery Care in the Ward
The first week following any major surgery tends to be bad in the sense of pain. I could do away with the bulky backslab post knee surgery, in exchange for leg braces. These had to be locked at 0 degrees for 6 weeks to prevent my knees from bending.
My white blood cell count tends to be low, which was a major concern to the Orthopaedic team. I was started on a course of prophylactic antibiotics to prevent any skin infections.
The surgeon and his team would change my dressing every few days to check on the wound. He would clean it with alcohol swabs without rubbing the skin as quickly as he could, to limit germs from entering the wounds.
My red blood cell count was also lower than my baseline, so the Orthopaedic team decided to give me a blood transfusion. As always, finding a single pack of blood for me is difficult as I am O negative with autoantibodies.
That is why I need to carry a medical card with me in my wallet stating so in case of an emergency. They had to filter the blood and hope that there would not be reactions.



Working with the Pain Management Team
The Pain Management team came to see me the next morning to see how they could help manage my pain better. As Pain Specialists, they understood the difference between drug addiction and drug resistance.
It’s a little tricky for me because I am also on psychiatric medications – a mix of mood stabilisers and antidepressants – that can interact with opioids.
As such, I can’t have too much opioid painkillers either for fear of Serotonin Syndrome, which can be deadly. As I had seemed fine from the single shot the night before, they decided to increase the fentanyl dosage.
Dealing with Serotonin Syndrome
Unfortunately, I started to get hot flushes and sweated so much that my clothing clung to my body. I was also running a mild feverish temperature. I recognised it to be a sign of Serotonin Syndrome and hurried to inform the doctors.
I requested for a fan to cool me down, a change of clothes, and a basin of water so that I could wipe the sweat off my skin and hair.
We had no choice but to reduce the dosage again, and I had to bear with the rest of the pain. We also contacted my Psychiatrist, who said that I could be taken off my psychiatric medications for a few days. She came to see me in the ward the following day to re-titrate my medications.
As a chronic illness patient we take so many medications, and each have the potential to interact with the other. A straightforward treatment for a healthy person is always complicated for us.
Pin to Your Knee Surgery & Chronic Illness Boards:
A Visit from the Physiotherapist and Occupational Therapist
Physiotherapists and Occupational Therapists play vital roles in injuries related to Orthopaedics, and also post surgery. To be honest, I didn’t know the difference between them prior to my knee surgery, but now their roles were crystal clear.
In short, a Physiotherapist (PT) aids a patient with physical rehabilitation. An Occupational Therapist (OT) on the other hand, teaches them how to execute everyday tasks following a physical impairment. It will be clearer with the examples of how they assisted me below.
The Start of Occupational Therapy
The OT explained the components of the wheelchair to me, and made sure I knew how to manoeuvre it in all directions. We went up and down the hallway a few times.
With the help of the nurses, we also found ways to safely transfer me from the bed to wheelchair and back, both sideways and backwards. I’d need at least three people to assist me, as my surgical wounds were still fresh and raw, and I had to keep my legs straight.
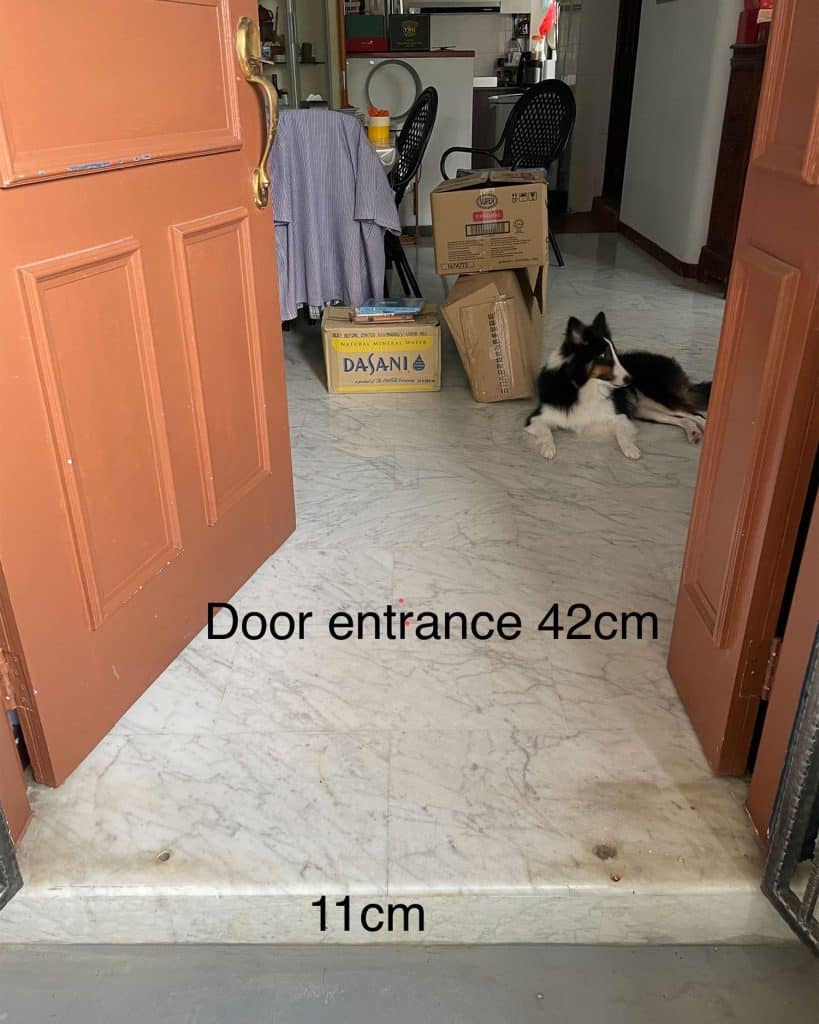
She asked questions about my home environment, such as if it had ramps or narrow spaces. She asked about the height of my bed, the structure of my room, and the size of my bathroom. She also recommended a wheelchair width based on my body size.
My parents snapped a few photos with measurements so she could have a better idea. We then discussed ways I could move around at home without provoking my knee injuries.
My parents were also busy back home renovating and rearranging my room to accomodate a hospital bed that someone kindly gave to us, and also for all the medical equipment I would need, such as a commode, leg braces and more. Our bathroom now has been completed revamped to be disability-friendly, too.
Limited Physiotherapy for Now
The PT on the other hand, examined the functionality of legs and feet, and asked where my pain was. She gave me a simple exercise to do – moving my feet up and down as much as I could.
The PT’s role would be more important further down the recovery timeline. For now there wasn’t much we could do for physiotherapy, as I had to keep my legs and knees totally flat for 6 weeks, to allow the tendons time to heal.
Pin to Your Knee Surgery, Physiotherapy & Occupational Therapy Boards:


The Difference in Rehabilitation Time for Single vs Bilateral Patellar Tendon Ruptures
Rehabilitation would be much different for a person who only suffered a patellar tendon rupture in one knee. Most would be able to start physiotherapy right the next day, in a bid to not let their leg muscles go to waste.
But when both patella tendons have ruptured and it’s impossible to stand or even lift your legs, then one has no choice but to let the muscles atrophy, in exchange for proper tendon recovery.
Besides, my knee tendons were apparently of poor quality no thanks to Lupus and steroids. So that was all the more reason to allow my patella tendons time to heal.
Week 2 – 3: Discharge from Hospital & Recuperation at Home
These were without a doubt, the toughest weeks in the whole recovery process. There is nothing you can actively do to help speed it up.
The best thing you can do to help yourself is to eat well and get plenty of sleep, to give your body the resources it needs to repair. You’ll probably be exhausted most of the time anyway. Recovery is hard work that takes place serreptitiously beneath the surface.
My mental health was at its lowest during this period of the recovery process. I was no longer amidst the hustle and bustle of the hospital, which helped with distraction.
There are no skilled nurses at home to assist with the disabled life, and our new helper wasn’t due to arrive until a week later. It was a trying week for my parents and me, as we navigated care around the clock. We were all sleep-deprived, at loggerheads and explosive.
It didn’t help that I had to leave my dog, Talisker, with some friends as he provides me with quite a bit of emotional support on a regular day. Although, my friends took such wonderful care of him and I couldn’t be more grateful!
The surgeon had actually suggested staying in a community hospital for a while, but I was adamant about going home. I have a huge phobia and dislike for hospitals and their routines. The surgeon acknowledge the mental toll it would take, and agreed to let me recuperate from home despite his concerns.


Struggling with Mundane Everyday Routines
Mornings are always hard for me because of chronic pain. It takes me about two hours every day to ‘wake up’, after my medications and lots of coffee.
Evenings are a little easier as we started to clean up and have dinner. I’d allow myself to watch some Netflix, and relax on the computer. Besides it was time to unwind and get ready to sleep.
Afternoons post lunch were the toughest part every day, where I’d sink into despair the most. There I was getting a sore ass in bed, locked flat in my leg braces and unable to move.
Every little knock against my legs that caused my knees to bend would make me cry out in pain. I had to travel via private ambulance for medical appointments as I couldn’t fit in a regular car with my legs stretched out.
Some of the paramedics were careless and presumed to know what to do, just because they had ‘years of experience’. They believed that just because my legs were locked in braces, I was entirely ‘safe’ from pain. False.
The Mental Challenge May be Harder to Deal with as Compared to the Physical
It was an extreme mental challenge as I’d repeat to myself, ‘whatever it takes to survive’, hour after hour, minute after minute.
My brain was still in shock as it had all happened so quickly. My life had taken such a drastic turn and I was lost. It was a place I’d never been to before. I had lots of experience with and knew how to deal with pain, but not the loss of physical independence.
I hated relying on others for the simplest of tasks, such as retrieving a pen on the table right next to me. I wasn’t able to shower as well, and those who read my blog probably know how much I love my showers.
I won’t rehash too much in this section, as I wrote an entire post on what it feels like to be suddenly disabled in this post.
Pin to Your Mental Health & Knee Surgery Boards:
Weeks 4 – 6: Laying Still Waiting for the Patella Tendons to Heal, Whilst Watching the Leg Muscles Atrophy
I had another 3 weeks to go before I could begin physiotherapy, but I felt a little better psychologically. I ordered some food as a small celebration the day we hit the halfway mark.
The leg braces were itchy, uncomfortable, heavy and affected the quality of my sleep. The surgeon granted me permission to remove them to sleep towards the end of this period.
Ironically, the quality of my sleep wasn’t much improved. The lack of mobility in my legs and knees meant that I couldn’t move my body much whilst asleep. This led to stiffness and aches in my neck and body every morning, on top of my ‘regular’ pains from chronic illness.
Afternoon naps were actually more restful, as I would sleep in a sitting position. So sometimes I sleep in that posture at night, too. I’ve changed my pillow many times but even supposedly ergonomic, expensive ones haven’t helped. I have yet to find a fix for this issue.
Finding Things to Occupy My Mind With, Whilst Allowing My Patella Tendons Time to Heal
By this point, my brain had had enough time to process the shock, more or less. By allowing myself to just be and to feel what I needed to feel, my heart and mind slowly started to heal, too.
My bosses are really supportive, empathetic and understanding people. They had continued to pay me, despite my lack of output during the past few months.
Now I was ready to dabble in a bit of work again. I also decided to learn some new things online. So I signed up for vocal lessons and took up French again online. It’s amazing how much you can learn and who you can connect with, through a small screen on the table!
In fact, I think my activities during this period was even more than before the bilateral patellar tendon rupture incident! I had a class or course slotted into nearly every day of the week. I usually feel flustered when my calendar appears to be packed, but this time I was happy that it was.
Distraction is crucial during this period, because there isn’t much you can do. Your knees need to just be, and you need to wait for them to heal at their own pace. Trying to speed up the process will only end in disaster.
My surgeon actually recommended that I find some engaging TV series, and to immerse myself in them for the next few months. So go ahead and gorge yourself on Netflix, if you like!

To be continued so stay tuned on my series about my Spontaneous Bilateral Patellar Tendon Rupture incident! (All the links are at the beginning of the post 😊)
Pin to Your Chronic Boards:

If you liked this article, sign up for our mailing list so you don’t miss out on our latest posts! You will also receive an e-book full of uplifting messages, quotes and illustrations, as a token of appreciation!
-
References:
- Bergman, R., & De Jesus, O. (2020). Patient care transfer techniques.
- Volpi-Abadie, J., Kaye, A. M., & Kaye, A. D. (2013). Serotonin syndrome. Ochsner Journal, 13(4), 533-540.
- Dean, L., & Dean, L. (2005). Blood groups and red cell antigens (Vol. 2). Bethesda: NCBI.

Sheryl, I’m so sorry to read how tough this journey has been for you so far, both physically and mentally. Thank you for sharing your story and journey to help others in a similar position know they’re not alone. I wish there was something I could do to make things easier. Just know I’m thinking of you and wishing you all the best for the rest of your recovery. Sending love and strength x